For a painless birth
The pain of childbirth has completely unique characteristics: it is limited in time and is immediately followed by the joy of the birth of the child.
However, for many women, the pain of childbirth is a significant obstacle. This fear absorbs a lot of energy and limits the possibility of a more active and serene participation in the birth of their child.

Labor analgesia. For some people, the suffering associated with childbirth is directly linked to the event of a new birth. For others, however, the true humanization of childbirth is achieved by reducing suffering and pain as much as possible. This is precisely the position from which modern obstetric analgesia derives.
It is possible to distinguish the different stages of labor, which are associated with more painful contractions:
Initial phase
The contractions have an irregular duration and the breaks between contractions vary. The pain is felt in the lower abdomen and/or in the lumbar area. In this stage, contractions can also disappear for a few hours.
Active phase
1. Dilation, in which the cervix is preparing for childbirth. In this phase, the pain is not precisely localized, but is felt in the umbilical region and lumbar area.
2. Expulsion, in which the child begins to descend through the birth canal. In this phase, the pain reaches its maximum and is well localized in the genital region and sacrum bone.
3. Delivery, which begins immediately after birth and ends with the expulsion of the placenta.
The greatest benefit of analgesia during childbirth is precisely the reduction of the mother's suffering. According to the World Health Organization and the most important American scientific societies of anesthesia (ASA) and ObstetricsGynecology (ACOG), "The request for analgesia by the woman represents in itself a medical indication for the treatment of pain during labor."
The analgesia techniques available at the Polyclinic of Milan are indicated below.
Pharmacological analgesia
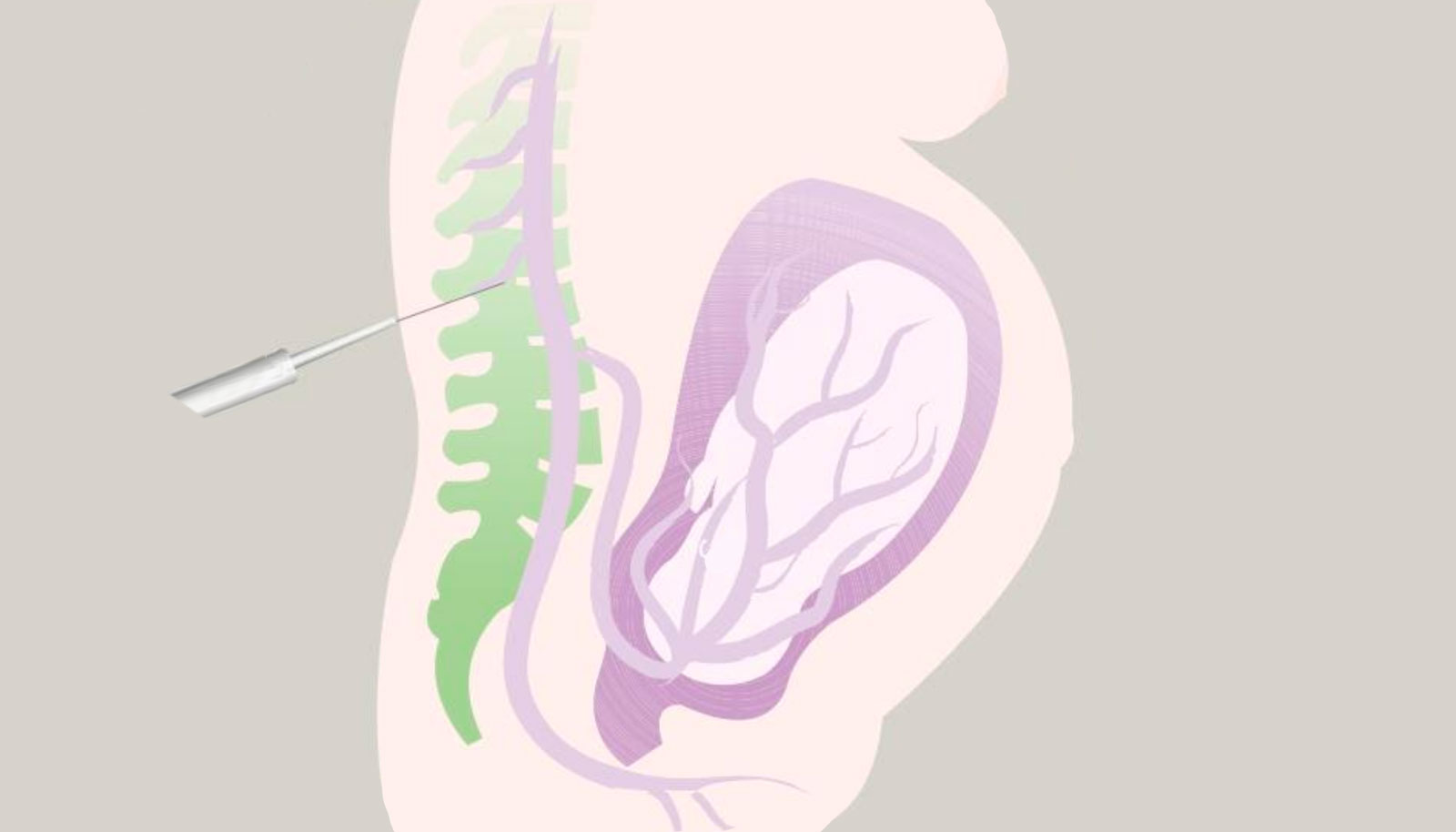
The advantage of the epidural route compared to other routes of drug administration is the fact that the analgesics injected into the epidural space (located near the spine) act directly on the nerves, allowing for reduced doses of anesthesia and therefore significantly reducing side effects, both in the mother and in the child.
This technique is also specifically indicated in all conditions where blood is struggling to reach the uterus and placenta (i.e., in the case of uteroplacental perfusion deficits) or in women with chronic diseases (e.g., heart disease, hypertension, respiratory diseases) who therefore have a high risk of peripartum complications.
Finally, if it is necessary to proceed with a cesarean section, the catheter already used for epidural analgesia can be used to perform surgical anesthesia, avoiding the use of general anesthesia.
Epidural allows 'walking'
Optimal epidural analgesia allows for normal movement of the woman, both during the dilation period and the expulsion period.
Absolute
• Coagulation disorders• Oral anticoagulant therapy
• Present sepsis
• Skin infections at the puncture site
Relative
• Tattoos in the area of the epidural needle insertion• Treatment with low molecular weight heparin or anticoagulant drugs, where there is no possibility of respecting the necessary suspension times.
• Specific pathologies, which will be individually analyzed based on the medical history and physical condition of the woman.
Epidural performed by expert and qualified personnel is a safe technique and
generally devoid of complications.
Immediate and transient side effects are represented by a sensation of warmth and
tingling in the lower limbs, a slight decrease in blood pressure (which is resolved by
administering intravenous fluids), and itching.
Post-analgesia epidural headaches occur in 1-1.5% of cases (1,2) and have completely
unique characteristics: they generally disappear with the supine position, are
controlled with common analgesics, and abundant fluid administration.
Variable intensity lower back pain may manifest after childbirth and is generally
more related to the complex dynamics of labor than to the positioning of the
epidural catheter.
Accidental dural puncture, a thin layer surrounding the spinal cord, can cause
headache due to the leakage of some of the fluid it contains. Post-analgesia
epidural headaches can occur in 1-1.5% of cases (1-3) and have completely unique
characteristics: they generally disappear with the supine position, are generally
controlled with analgesics, caffeine, and abundant fluid intake. The need for patient
blood injection at the same site of positioning is rare, but if it occurs, it can lead to
infection or nerve damage.
Serious neurological complications that are certainly attributable to the technique are decidedly rare; their incidence varies between 0.3 and 1.2 cases per 100,000 epidural analgesia performed (4).
1. Van de Velde M. Schepers R. Berends N et al (2008) Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia deparment. Int J Obstet Anesth 17(4):329-335
2, Choi PT, Galinski SE, Takeuchi L et (2003) PDPH is a common complication of neuraxial blockade in parturients: a meta-analysis of obstetrical studies. Can J Anaesth 50:460-469
3. Costa AC, Satalich JR, Al-Bizri E et al (2019). A ten-year retrospective study of post-dural puncture headache in 32,655 obstetric patients. Can J Anaesth. 66:1464-1471
4. Cook TM, Counsell D. Wildsmith JAW, Royal College of Anaesthetists Third National Audit Project (2009) Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth 102:179-190
After the sixth month of pregnancy, an anesthesiology visit should be scheduled to
identify specific issues or potential contraindications. As a medical procedure,
during a preventive interview, specific information related to the proposed technique
is provided, and if any risk conditions are identified, they are discussed in a phase
of psychological calmness for the expectant mother.
On the day of delivery, analgesia can be requested upon entering the delivery room
or when labor begins by informing the obstetric team, who will then inform the on-
duty anesthesiologist. Upon arrival, the anesthesiologist will review the maternal
conditions from the previously conducted outpatient visit, verify the hematological
and biochemical tests already performed (hemoglobin, prothrombin time, activated
partial thromboplastin time, and fibrinogen), and require written consent for the
procedure.
It should be noted that the validity period for these tests is one month before the
due date.
The administration of analgesia will be performed as quickly as possible
or within 60 minutes of the gynecologist's visit, who during active labor must
exclude any obstetric contraindications to the procedure, which often represents an
indication for a cesarean section.
On the day of birth, analgesia may be requested upon entry into the delivery room or once labor has started.
To schedule an appointment for the anesthesiology visit:
Between the 28th and 37th week of pregnancy - follow these instructions
www.policlinico.mi.it/mangiagalli-center/diventare-mamma/calendario-visite-e-esami-gravidanza#step12
Anesthesiology Visit (epidural analgesia/anesthesia)
Women who choose to give birth at the Mangiagalli Clinic (spontaneous delivery) must undergo the anesthesiology visit. The visit allows the woman to request epidural analgesia during labor. The assessment by the obstetrician-gynecologist and the anesthesiologist determines the timing for the procedure.
In order to book the Anesthesiological visit:
Follow these instructions
www.policlinico.mi.it/mangiagalli-center/diventare-mamma/calendario-visite-e-esami-gravidanza#step25
Aggiornato alle 09:01 del 09/02/2024


